Pelvic organ prolapse is as old an ailment for women as mankind itself. Since the time human beings attained upright posture, gravity has played a part in the appearance of prolapse.
Almost 10% of young women and 50% of postmenopausal women may develop prolapse in their lifetimes. The fact that this is a disorder most women don’t even know they have, it becomes more important for us to understand what it means.
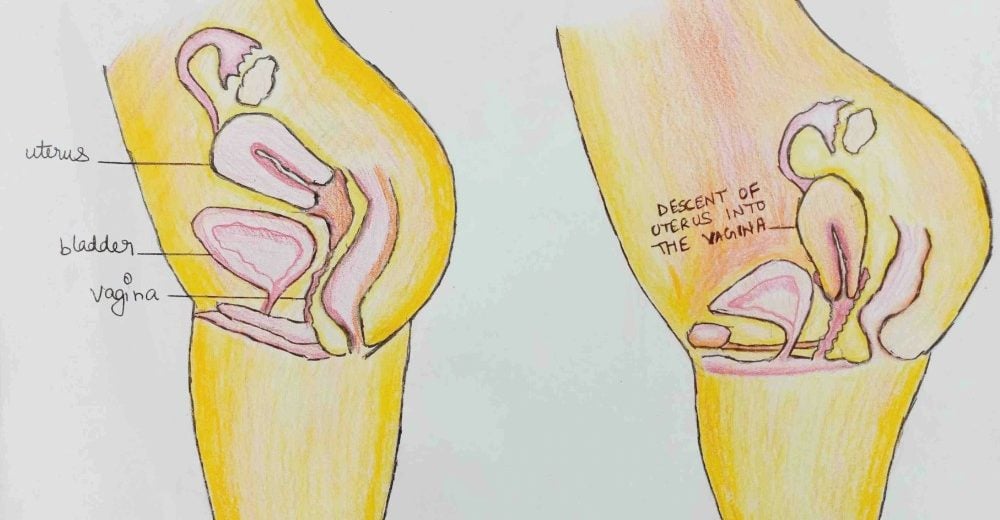
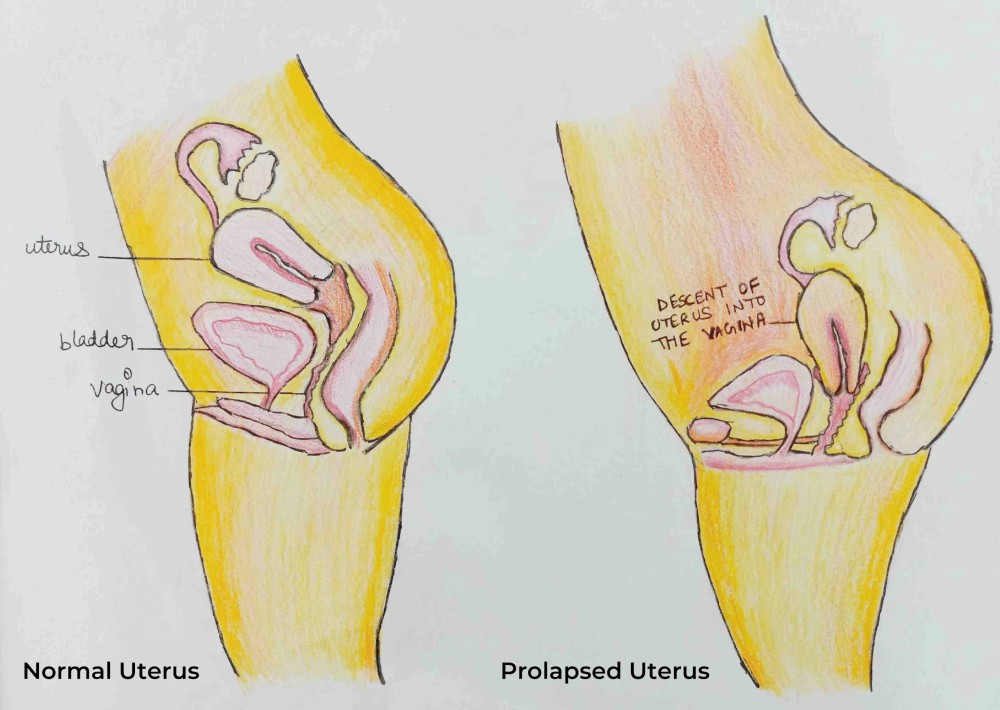
Prolapse is a pelvic floor disorder. When the pelvic floor muscles and ligaments responsible for supporting a women’s pelvic organs become weak, the organs start dropping down into the pelvis region and bulge into the vagina.
But how does all this happen?
“Your pelvic organs entail the uterus, bladder, rectum and vagina. These organs are held in place by the pelvic tissues and ligaments and are given support from below by the pelvic floor muscles. When these ligaments and tissues get stretched or torn and the muscles are no longer strong enough to give support to the organs, they start sagging down into your vagina,” explains Dr. Namrita Gurpal Singh Sandhu , Consultant Gynaecologist and Obstetrician at Sitaram Bhartia Hospital.
“Prolapse isn’t a life-threatening condition but it can deteriorate your quality of life tremendously.”
What leads to a pelvic organ prolapse?
There are certain factors that could put you at risk of experiencing a prolapse:
- Pregnancy and childbirth – Pregnancy and childbirth may occasionally take a toll on your pelvic region. It may cause the pelvic muscles to stretch and tear as a result of which they might loosen up and increase the risk of prolapse.
- Aging and Menopause – As you approach menopause, the estrogen levels in your body often decrease. Since estrogen helps strengthen the pelvic muscles, lower quantities of estrogen may lead to an increased chance of a prolapse.
- Obesity – As the body becomes heavier due to obesity, your abdomen starts exerting more pressure on the pelvic organs. This forces them down towards the vagina leading to prolapse.
- Chronic constipation – Constant straining to allow bowel movement may put pressure on the pelvic muscles and loosen them.
- Chronic cough – Similar to constipation, coughing for a long period of time can put strain on the pelvic floor muscles making them weak.
What are the signs and symptoms of prolapse?
The symptoms that a woman might experience when she has a prolapse depends on the type of prolapse and the extent to which the organ has bulged into the vagina.
Some common symptoms that you might experience are:
- Feeling of something heavy pushing down your vagina and lower abdomen.
- Feeling a bulge protruding out of your vagina.
- Discomfort during sex.
- Inability to empty bladder completely.
- Frequent urge to pass urine.
- Difficulty in starting urination or passing bowel.
- Leakage of urine while coughing, sneezing or exercising.
Prolapse – How is it diagnosed?
People who have prolapse often come with complaints of symptoms like a feeling of heaviness in their vagina or something coming out of it.
A physical pelvic examination is done to see whether any organ is protruding out of the vagina.
“We also take into account the patient’s medical history.”
What are the different ways in which prolapse can take place?
(i) Prolapse may sometimes appear as a bulge protruding out of the cervix. This is the uterus or a part of it coming out of the vagina. It happens when the pelvic floor muscles are no longer able to give support to the uterus causing it to slip down.
“Postmenopausal women, especially those who have had one or more deliveries, are more at risk of having a prolapsed uterus. But this condition can happen to women of any age,” remarks Dr. Namrita Gurpal Singh Sandhu.
(ii) At times the bladder starts protruding along with the front wall of the uterus. This takes place when the pelvic fascia between the vagina and the bladder become weak and the bladder starts sagging into the vagina.
“Women display mild symptoms when the bladder drops only a short way into the vagina. When it starts protruding through the vaginal opening, severe symptoms surface which may cause discomfort and pain as well.”
(iii) When the back wall of the vagina becomes weak, your rectum i.e. the last section of your large intestine slips down from its normal position and bulges out of the vagina, it’s referred to as rectal prolapse. It is a common pelvic floor disorder in older women especially those who may have experienced chronic constipation or cough.
Apart from the common risk factors of developing prolapse, certain conditions such as diabetes, cystic fibrosis, COPD and hysterectomy may also lead to this type of prolapse in women.
How can a prolapse be treated?
“Several treatment options are available for prolapse but it all depends on the type and the extent of it.”
Mild symptoms of prolapse often don’t require conventional treatment modalities. They can be very well managed with a couple of lifestyle changes like:
- Doing regular pelvic floor exercises: Kegel exercises (especially after childbirth) can help strengthen the pelvic muscles when done on a daily basis.
- Preventing or treating constipation: As constipation puts pressure on your pelvic muscles and makes your prolapse worse, it’s good to get it treated. A high-fibre diet consisting of spinach, pulses and fruits also helps prevent constipation.
- Losing weight
- Quitting smoking
- Avoiding lifting heavy objects on a daily basis
Some postmenopausal women having mild prolapse symptoms may be suggested an estrogen treatment due to lack of this hormone in their bodies.
“Estrogen can be given in the form of a cream or tablet to be inserted in your vagina,” says Dr. Namrita Gurpal Singh Sandhu.
Other treatment options
Vaginal pessaries – Vaginal pessaries are devices made of rubber or silicon which are inserted into your vagina to provide support to it and to hold the pelvic organs in place. These are generally used for women showing moderate to severe symptoms which are disrupting their daily life.
Surgery – In case your symptoms are too severe to be managed with non-surgical options, surgery can be used to correct the prolapse.
“Surgical treatment involves lifting and giving support to the pelvic organs by either stitching them in place or by making the tissues stronger. Cystocele i.e.bladder prolapse, if associated with urine leakage, may need to be treated by putting a tape to hold up the bladder neck.”
Prolapse is a condition which can affect women of any age but if you make the right lifestyle choices, you can reduce the chances of developing it.
Seek expert advice from our Gynaecologist. Please call on +91 9871001458 to schedule a consultation.
 Medically Reviewed by Dr. Namrita Gurpal Singh Sandhu
Medically Reviewed by Dr. Namrita Gurpal Singh Sandhu
MBBS, Government Medical College & Hospital, Chandigarh, India (2005) DNB, National Board of Examinations (2012), MRCOG (Part One), Royal College of Obstetricians and Gynaecologists (2015), Diploma in Gynecological Laproscopy, Hysteroscopy and Urogynecology, Kiehls school, Germany (2019)
Experience: 10+ years