During pregnancy some expecting women may not be able to cope with the increased insulin requirement. This may result in a need to take insulin during pregnancy.
For first-time mothers and especially women who did not have diabetes before pregnancy, this can be a stressful and frightening situation.
Priya Kashyap for example was counselled about gestational diabetes in her third month.
“I was taken aback at first,” she says, “but my diabetes care team explained that I could control gestational diabetes by changing my diet and exercise routine.”
“I made a conscious effort to walk for 45 minutes every day and included proteins, whole grains and green vegetables in every meal.”
“I was also particular about monitoring my blood sugar levels as advised by the diabetes team.”
“Despite all these efforts and medication, my blood sugar levels did not decrease. I was then recommended insulin during pregnancy.”
What is Insulin?
Insulin is a hormone that is released by the pancreas. This hormone converts the glucose in the blood to energy that is used by the cells for body functions.
In Type 2 diabetes, your body may become insulin resistant – meaning that glucose or blood sugar is not being used up by the cells properly even though the pancreas produces insulin.
In gestational diabetes, your body will not produce enough insulin to meet the additional needs during pregnancy and it will not be effectively utilized (insulin resistance). As a result, you will have high blood sugar levels.
When should a pregnant woman take insulin?
You will be advised insulin during pregnancy if diet, exercise and medication have not helped reduce your blood sugar levels to these target levels:
- Fasting blood sugar <92 mg/dl
- 1 hr post meal< 140 mg/dl
- 2 hr post meal <120 mg/dl
- premeals<95 mg/dl
Those with Type 2 diabetes will need to switch to insulin when they conceive as many oral medicines are not considered safe because of their potential to cross the placenta and reach the baby.
How does insulin affect a fetus?
Insulin is a very safe choice in pregnancy as it does not cross the placenta and reach the fetus.
Explaining the condition, Dr. Silviya Irene, Consultant Endocrinologist at Sitaram Bhartia Hospital says “ When the mother does not meet the insulin requirements, the high glucose levels in the blood get transmitted to the baby through the placenta. Higher than normal levels of glucose can cause babies to become bigger and may cause other complications.”
“The only way to provide additional insulin is through injections. When the mother takes these injections, the glucose is disposed off in a proper manner to provide energy. This prevents the excess glucose from reaching the baby and averts any complications.”
Types of insulin
Insulin is available as an injection. There are different kinds of insulin based on how fast they act, the peak time (at which it is highest in the blood) and the duration or length of time for which it continues to lower blood sugar levels.
“The type of insulin appropriate for you depends on your blood sugar levels,” says Dr. Silviya.
- Rapid-acting insulin which should be taken 10-15 minutes before meals as it works within 15 minutes and peaks in 1-2 hours. It’s effect lasts for 3-4 hours.
- Short-acting insulin which works within 30 minutes, peaks in 2-3 hours and lasts for 3-6 hours.
- Intermediate-acting insulin which works within 2-4 hours, is at maximum strength in 4-12 hours and lasts for 12-18 hours.
- Long acting insulin which works after 2-3 hours but lasts for 24 hours.
“I had many misconceptions about insulin during pregnancy which were patiently cleared by the diabetologist and educator,” remembers Priya.
“They took the time to answer all my questions about insulin in pregnancy guidelines, dosage, when to take insulin and how much insulin I should take during pregnancy..”
How Much Insulin Should Pregnant Women Take?
“The dosage and the type of insulin depend on your weight, gestation period, diet and glucose profile,” says Dr. Silviya.
Where should a pregnant woman inject insulin?
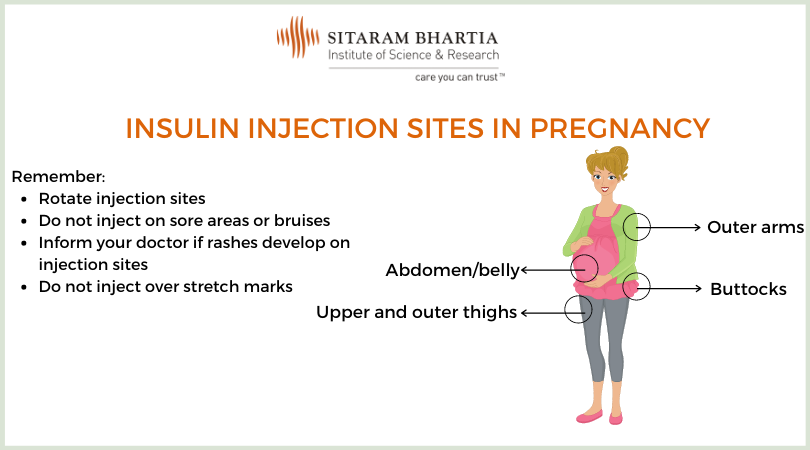
Pregnant women should inject insulin in areas rich in fat mass such as the abdomen or sides of the thigh as insulin is best absorbed in these areas. This is less painful and helps absorb the insulin faster. Some injection sites/areas are:
- Abdomen/belly or two inches away from the belly button
- Outer side of the arms that contain more fat
- Upper and outer side of the thighs
- Outer side of the buttocks
Tips for Selecting Insulin Injection Sites
- Avoid areas that have bruises or injection sites where you develop bumps or soreness as the insulin will be absorbed differently and will affect your blood sugar levels.
- Avoid using an area that you are likely to exercise as that could cause insulin to be disposed much faster.
- Rotate sites by selecting an area in a way that there is atleast a one finger breadth between two insulin shots. If you notice a bump or nodule at the injection site, it is better to avoid the site as the insulin absorption could be erroneous.
- Note any rashes at the injection site as this may indicate an allergy or infection; do not use this area for a few months until after the infection is treated.
“The thought of taking an injection everyday was intimidating, so I was very glad that I took the first shot in front of my doctor under her supervision. That gave me confidence,” says Priya.
How do you inject insulin while pregnant?
You can follow these steps when using most types of insulin pens:
- Wash your hands and collect your insulin pen, needle, alcohol swabs and a container for the needles
- Uncover the pen and clean the top of the pen with an alcohol swab
- Open the needle by peeling off the cover and placing it on top of the pen; remove the outer covering and the needle cap
- Turn the knob in the pen to a unit; push the injection button; when you see the insulin coming out, you will know that the pen is ready to use
- Turn the knob in the pen to ensure you have the correct dosage of insulin
- Clean the injection site with an alcohol swab and then inject the needle firmly at a 90 degree angle. Pull it out after 5-10 seconds.
Watch a video with instructions to use an insulin pen.
Tips for taking insulin during pregnancy
- Change insulin sites to prevent soreness from repeatedly using the same area; move an inch or two away from the original site
- Inject insulin at the same time every day; if you feel unwell, inform your diabetes specialist
- Consult your doctor before altering your exercise routine or diet
- Store the bottle of insulin (that is being used currently) at room temperature
- Track the amounts of insulin you are taking, especially if you take two different types
- Dispose the needle in a container meant for sharp objects that is separate from other waste
Are there any side effects of taking insulin during pregnancy?
The main insulin side effect during pregnancy is that it could cause low blood sugar levels (hypoglycemia) in case you missed/delayed a meal or injected excess insulin.
“My doctor alerted me of the signs to watch out for and how to treat low blood sugar during pregnancy,” says Priya.
What are the symptoms of low blood sugar in pregnancy?
If you are hypoglycemic or your blood sugar is low (70 mg/dl ), you may experience these symptoms:
- Sweating, dizziness, feeling shaky
- Feeling faint
- Blurred vision
- Palpitations
- Tremors
- Hunger
The quickest way to treat the condition is to have a spoon of honey or a few raisins (kishmish) or some fruit juice and raise your blood sugar levels.
“I was constantly reminded that I have to keep checking my glucose levels throughout the day and maintain a record,” shares Priya.
Tips to Monitor Blood Sugar Levels While Taking insulin during pregnancy
- Check your blood glucose levels 6 times a day.
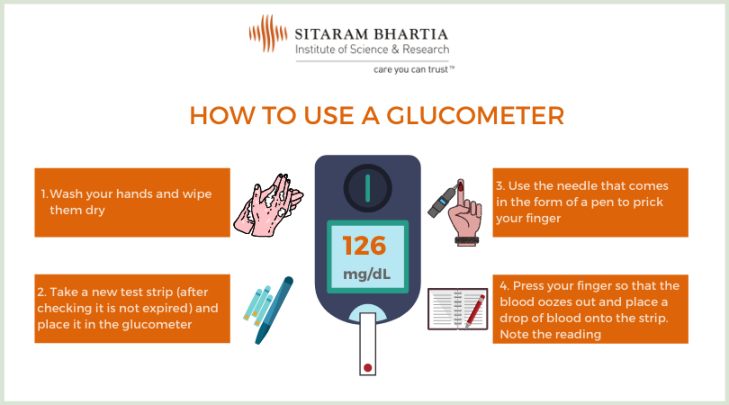
“You may have to check your blood sugar less or more often depending on your glucose profile,” says Dr Silviya. - Use a glucometer to monitor your blood sugar levels easily.
Read: PPBS Test: 3 Practices That Affect Your Results
- Visit your diabetes care team as advised as each consultation helps monitor your progress and determine whether any changes to your treatment plan are needed
“I think my gestational diabetes was well-managed because the doctor and educators kept such a close watch on my diet, exercise and blood sugar levels. Their aim is to control diabetes in the short-term and to prevent it from returning in the future.”
“It was because of their constant guidance that I eventually had a safe normal delivery, which was a big deal for me,” finishes Priya.
Hear Priya Kashyap’s full gestational diabetes journey here:
Q&A Common Questions on Taking Insulin During Pregnancy
Q. Is it ok to inject cold insulin?
A.You could use cold insulin but it will be more painful so you should bring it to room temperature before using it.
Q. How do I store insulin?
A.You can store unopened bottles of insulin in the refrigerator door; but do not keep them in the freezer or in direct sunlight as extreme temperatures affect insulin. Always check the expiration date before using the insulin.
Store an open bottle of insulin at 8 to 20 degree celsius for no longer than a month, else it will not be fit for use.
Take out a new bottle of insulin from the fridge well before you prepare your injection so that it can warm up to room temperature.
Q. Is there another way to measure your blood sugar apart from pricking yourself several times a day?
A.You could use a sensor that is placed on your body and gives 24 hour blood sugar readings.
The set of readings or ambulatory glucose profile (AGP) is checked in your doctor’s office when you return after 14 days. It gives insight into how your blood sugar levels change depending on your meals and physical activity.
Q. Do I need to continue taking insulin during pregnancy, labour and delivery?
A.On the day of delivery and at the time of labour, the need for insulin will depend on the blood sugar levels at that time. The blood sugar levels generally improve after delivery and insulin levels are gradually tapered.
You should check for diabetes (blood sugar fasting and 2 hours after 75 gms of glucose) 6-13 weeks after giving birth and every year after that even if the result is normal, especially if you plan to have another child.
If you are unsure of how to navigate your pregnancy with diabetes, don’t hesitate to come in for a complimentary consultation at our hospital in South Delhi. Please call +919871001458 to schedule your complimentary consultation.
This article has been written with editorial inputs from Dr. Silviya Irene who is known to be passionate about endocrinology and helping expecting women manage gestational diabetes in the best possible manner.
 MBBS, Tamil Nadu Dr. M.G.R. Medical University, Tamil Nadu (2005); Diploma in Diabetology, Tamil Nadu Dr. M.G.R. Medical University, Tamil Nadu (2008); D.N.B (General Medicine), National Board of Examinations (2012); Senior Residency in Endocrinology from Safdarjung Hospital
MBBS, Tamil Nadu Dr. M.G.R. Medical University, Tamil Nadu (2005); Diploma in Diabetology, Tamil Nadu Dr. M.G.R. Medical University, Tamil Nadu (2008); D.N.B (General Medicine), National Board of Examinations (2012); Senior Residency in Endocrinology from Safdarjung Hospital