Have you been experiencing persistent stomach pain or weight loss that is hard to explain?
Inflammatory Bowel Disease (IBD) is a condition that not only affects the gut but has an impact on the overall health of a person. In women, however, it impacts much more than that.
Let us know more about this condition and how it impacts a woman’s health.
What is Inflammatory Bowel Disease?
Dr. Nivedita Pandey, Consultant Gastroenterologist at Sitaram Bhartia, explains, “Inflammatory Bowel Disease or IBD is an umbrella term used to describe conditions that cause chronic inflammation in the digestive system.”
“By inflammation we mean that any part of the digestive tract becomes red and swollen causing uncomfortable symptoms in the body.”
Inflammatory Bowel Disease mainly comprises two conditions –
- Ulcerative Colitis
- Crohn’s Disease
This disease can happen to anybody but is more common in people between 15 and 40 years of age.
“In women, IBD affects their menstrual cycle, fertility, pregnancy and menopause in some way or the other,” Dr. Nivedita comments.
Inflammatory Bowel Disease symptoms – How do I know if I have IBD?
There are some common symptoms that people having any of the two diseases might experience. These are –
- Recurrent diarrhea, often with blood or pus
- Severe and persistent abdominal pain or cramping
- Rectal pain
- Blood in stool (rectal bleeding)
- Sudden urges to pass stool
- Inability to defecate despite urgency
- Loss of appetite followed by weight loss, fatigue and fever
Dr. Nivedita says, “The point to note here is that in case of IBD, symptoms tend to come and go. People will experience long periods of time when they’ll have no symptoms at all. This is known as remission period when the disease is inactive. But they will go through episodes of flare-ups where the symptoms will reappear and the disease will be active again. “
Let us understand these two conditions under IBD in detail.
Ulcerative Colitis
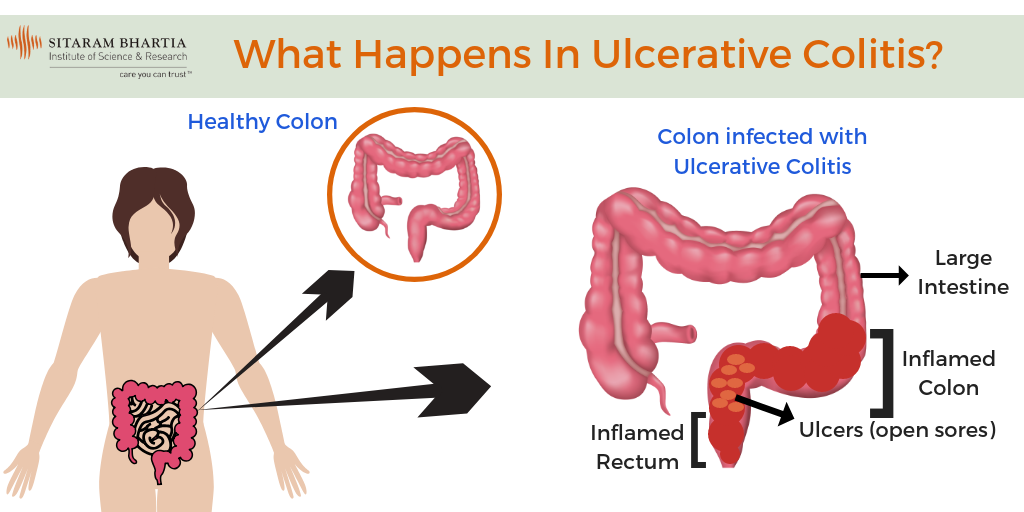
Ulcerative Colitis is an inflammatory bowel disease that causes chronic inflammation in the large intestine or colon and the rectum (last section of the colon).
Read: Ulcerative Colitis in Hindi
It inflames the innermost lining of the colon leading to the formation of ulcers or open sores. These ulcers may also produce pus and mucous leading to abdominal discomfort.
Crohn’s Disease
Crohn’s Disease is an IBD that can cause inflammation in any part of the digestive tract – from the mouth to the anus.
“In this condition, the inflammation can spread deep into the affected tissues causing severe damage to that part of the digestive system,” Dr. Nivedita says.
“The main difference between Ulcerative Colitis and Crohn’s Disease is that Ulcerative Colitis affects only the colon and rectum whereas Crohn’s Disease can affect any part of the digestive system.”
Symptoms experienced are almost the same in both the conditions.
As Crohn’s Disease causes inflammation that goes deep into the tissues, it leads to a few complications like –
- Bowel obstruction: Crohn’s Disease affects the thickness of the intestinal wall. Over time, certain parts of the bowel get scarred and narrowed due to the inflammation. This blocks the natural movement of the bowel.
- Fistulas: Fistulas are basically tunnels that abnormally connect different body parts. The inflammation caused can lead to the formation of ulcers. These ulcers may expand through the intestinal wall forming fistulas. These fistulas can develop between the intestine and vagina or bladder.
- Anal fissures – In severe instances of Crohn’s Disease, small tears may develop in the lining of the anus. These are known as fissures. People with anal fissures experience pain while passing stool.
- Colon cancer – In situations where Crohn’s Disease and Ulcerative Colitis affect the colon there are increased chances of developing colon cancer.
But the question still remains – what causes these chronic inflammatory diseases?
What causes inflamed bowel disease?
The exact cause of Inflammatory Bowel Disease is unknown but there are certain theories that may explain why some people develop it:
Abnormal immune response – IBD is sometimes said to be caused by an abnormal response of the immune system.
Family history – People with a family history of IBD have higher chances of developing it themselves.
Women and Inflammatory Bowel Disease – FAQs
Inflammatory Bowel Disease is a chronic condition which impacts women and their reproductive health.
Dr. Nivedita says, “Women with IBD come to me with a lot of questions regarding their menstrual cycles, pregnancy and post-menopausal life.”
Some of these questions are addressed below –
How does having Inflammatory Bowel Disease affect my menstrual cycle?
“Menstrual cycles tend to become irregular with IBD. This happens because the menstrual cycle gets affected by many factors such as the hormone levels in the body, proper nutrition and stress levels. In IBD, due to the inflammation, the body is unable to absorb nutrients it needs to function properly. This lack of adequate nutrition causes the body to shut down which causes an improper functioning of hormones which then affects the menstrual cycle,” Dr. Nivedita explains.
Can I get pregnant naturally with Inflammatory Bowel Disease?
IBD hardly impacts a woman’s fertility.
In case of Crohn’s Disease, sometimes women have to undergo extensive surgery to relieve the symptoms. This increases the risk of infertility due to development of scar tissues.
“If you have IBD, it is advisable to consult a doctor before you try to conceive.”
What happens if I get pregnant with Inflammatory Bowel Disease?
The nature of the disease during pregnancy depends on its state before pregnancy.
Dr. Nivedita explains, “What this means is that if your IBD was inactive before you became pregnant i.e. you were in your remission period then it is likely that your disease will remain in remission during the course of pregnancy. If you become pregnant while your disease is active (flare-up period) then it is likely that your symptoms will continue or may become worse.”
“That’s why I recommend my patients to try conceiving while their disease is inactive.”
How will Inflammatory Bowel Disease affect my baby during pregnancy?
Women, who become pregnant while their disease is active, have higher chances of developing complications like fetal loss or preterm birth.
According to Dr. Nivedita, “A baby’s growth and development depends on the state of IBD and its severity during pregnancy. It also depends on the treatment methods adopted during that time.”
“A pregnant woman with IBD should be under the care of both a gastroenterologist and an obstetrician to ensure that both the mother and her baby are healthy during the gestation period.”
How does Inflammatory Bowel Disease affect menopause?
IBD doesn’t have any significant effect on menopause.
“A woman with IBD, who is also going through menopause, hasa higher risk of developing bone problems like osteoporosis. This is due to the lack of adequate nutrition in the body which takes a big hit after menopause.”
Inflammatory Bowel Disease Treatment – How to treat IBD?
There is no permanent cure either for Ulcerative Colitis or for Crohn’s Disease.
“Treatment for IBD usually focuses on relieving the symptoms and prolonging the remission period so that people stay symptoms-free for longer periods of time. This can be done by reducing the inflammation through some lifestyle and dietary changes along with medication. Surgery is suggested when the disease becomes more severe,” Dr. Nivedita says.
Medication
- Anti-inflammatory medicines: This is the first step in treating IBD. They help in reducing the inflammation in the affected area.
- Immune system suppressors: These medicines focus on reducing the activity of the immune system that causes the inflammation.
- Antibiotics: These help in relieving symptoms.
Lifestyle and Dietary changes
- Keep a close eye on what you eat and which food items aggravate your symptoms. Try avoiding those food items.
- Limit or avoid the consumption of alcohol.
- Eat small meals 5 to 6 times a day instead of having 3 big meals.
- Consume plenty of water on a daily basis.
- Avoid smoking. It will make the symptoms worse.
- Exercise regularly. This will help manage stress and normalize your bowel movements.
Surgery
“We advise surgery only when the condition becomes very severe and symptoms can’t be managed with medication,” Dr. Nivedita says.
In case of Ulcerative Colitis, when the entire colon and rectum get severely damaged, they are removed through surgery. A pouch is then created using the end of the small intestine. It is then attached directly to the anus allowing the patient to expel waste normally.
In Crohn’s Disease, surgery is often required to remove the damaged sections of the digestive tract and reconnect the healthier sections to allow proper bowel movement.
Surgery may also be advised to treat complications that arise in Crohn’s Disease like fistulas and fissures.

